Abstract
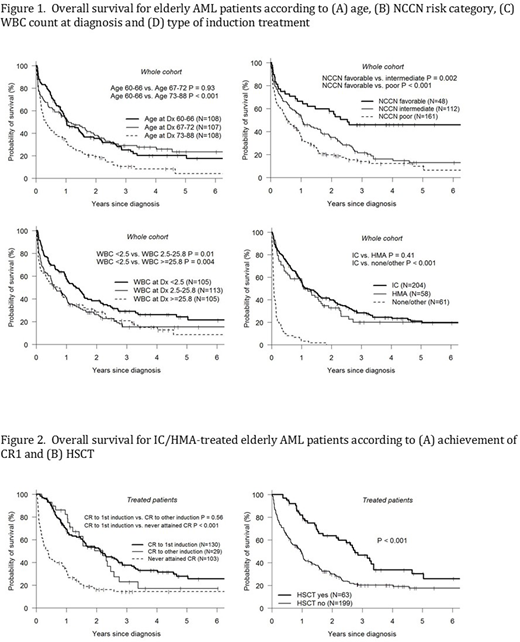
The median age of acute myeloid leukemia (AML) diagnosis is 69 years with 60% of newly diagnosed patients > 60 years. Due to a perceived intolerance to therapy, many elderly AML patients do not receive therapy. Of those that do, few are eligible for curative intent therapy with hematopoietic stem cell transplantation (HSCT) due to perceived lack of fitness, excessive comorbidity or absence of a donor. To better understand the outcomes of elderly AML patients, we evaluated a cohort of 323 consecutive elderly AML patients (≥60 years) referred to the Leukemia Program at Northside Hospital from January 2009 to December 2017 for evaluation and management. Our treatment algorithm is to offer intensive chemotherapy (IC) to all potentially eligible patients and HSCT to all transplant-eligible non-favorable risk patients that achieve complete remission, with or without complete platelet recovery (CR1(p)). Median patient age was 70 years (range 60-88). AML occurred de novo in 218 (67%), therapy-related in 33 (10%) and secondary in 72 (22%) patients. NCCN risk category was favorable (fav) in 48 (15%), intermediate (int) in 112 (35%) and poor in 161 (50%). Leukemia induction therapy, either IC (n=204) or hypomethylating agents (HMA, n=58), was given to all but 61 (19%) patients (IC - 78%, HMA - 22%). Of patients receiving IC, the major regimens were FLAG+/-Ida (n=117), 7+3 (n=58) and CPX-351 (n=18). Of the IC/HMA-treated patients (n=262), 130 (50%) achieved CR1(p) with the first induction, while 158 (60%) ultimately achieved CR1(p). In patients with fav, int and poor risk AML, CR1(p) was achieved in 73%, 52% and 41% respectively. HSCT was performed on 63 patients (59 - int/poor risk, 4- fav risk): autologous [5], matched sibling donor [21], matched unrelated donor [24], haploidentical donor [13]. Of the non-fav risk AML CR1(p) patients, where the treatment goal is HSCT if feasible, 57 (46%) of 124 received HSCT. After a median f/u of 34 months, 2-year overall survival (OS) for the whole cohort was 31%; corresponding rates for fav, int and poor risk AML was 58%, 35% and 20% respectively. Survival was similar in patients aged 60-66 and 67-72 years (2-yr OS 35% and 38%), but superior to those in the 73-88 yr tertile (2-yr OS 19%, p<0.001). The 2-yr OS was similar for IC- or HMA-treated patients (40% and 33% respectively) vs. 0% for patients not receiving induction therapy. For patients achieving CR1(p), 2-yr OS was 50% vs. 16% for those never reaching CR1(p). Of the patients receiving HSCT, 2-yr OS was 64%. In the subset of non-fav risk AML CR1(p) patients, OS was improved with HSCT (p<0.001, 2-yr OS 66% vs. 27%). In multivariate analysis, we analyzed factors associated with mortality including age, gender, race, year of diagnosis, WBC, de novo vs. secondary, NCCN risk category, and induction chemo type (receipt of HSCT was not analyzed given inherent bias in such as analysis). Factors associated with superior OS included WBC <2.5 at diagnosis (2.5-25.7, HR 1.92, p<0.001; ≥25.8, HR 1.93, p<0.001), NCNN fav risk (int, HR 2.02, p=0.002; poor, HR 2.71, p<0.001) and receipt of either IC or HMA induction (no induction vs. IC, HR 7.65, p<0.001; HMA vs. IC, HR 1.20, p=0.315). With the caveat that any such analysis is subject to referral bias, these results suggest that survival may be improved in elderly AML patients through a coordinated approach of remission induction therapy followed by HSCT when feasible.
Solh:Celgene: Speakers Bureau; Amgen: Speakers Bureau; ADC Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal